How do we take care of you?
COMPREHENSIVE VIEW
Advice in Clinical Oncology was developed to meet the needs and rights of the patient. It begins with a comprehensive assessment of the functional, emotional, cognitive and social impact of the disease on patient and families’ lifestyle. Personalized care combines proficiency with sensitivity. Cognitive psychology resources are used to improve empathy, expressed in detailed description of diagnosis and treatment, using clear and accessible language. Technical recommendations follow international criteria, supported by levels of evidence, and are always subject to patient’s shared decision-making. Emotional barriers are overcome through a direct and qualified doctor-patient relationship. A new steady state is created, leading to progressive recovery of self-esteem, reorganization of family dynamics and resumption of daily activities.
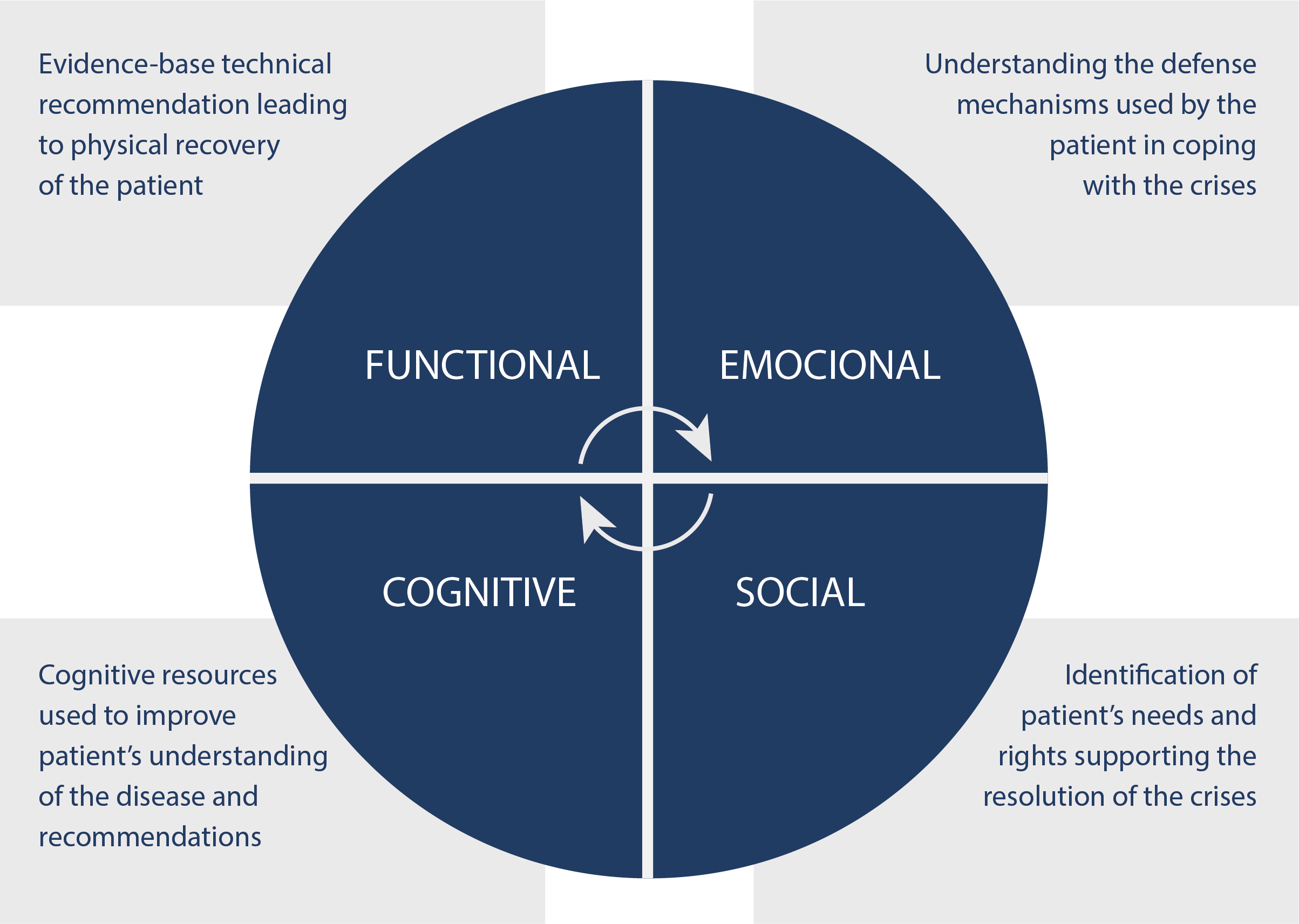
Illness is always an unexpected event. Although the initial complaint is often physical, the extent of the damage goes far beyond functional limitations. Human sensitivity is proportional to its complexity. Medicine only fully achieves its objectives with a multidimensional integrative approach. The figure shows how we deal with functional, emotional, cognitive and social consequences imposed by illness. This is not an isolated medical intervention, but an ongoing professional practice, modulating patient and families’ dynamics. Gradually a new steady state is achieved based on mutual trust, cooperative behavior and proactivity.
Respecting patient’s needs and rights restores their self-esteem and creates a new state of balance
We provide a customized care, combining proficiency with sensitivity
BEHAVIORAL AND ENVIRONMENTAL CHANGES
Our care model involves behavioral and environmental changes, removing any type of professional barrier that prevents free communication with the patient. This includes any physical or emotional obstacles placed between the doctor, the patient and the family, which may block spontaneous dialogue. The consultation takes place in a living room, where the doctor, the patient and the family sit in comfortable chairs, assuming a circular arrangement and creating a relaxed environment. The goal is to exercise belonging, better understanding the patient’s complaints and adopting a cognitive approach. The presence of family members is encouraged, as our care model works with the patient-family binomial. The doctor does not wear a white coat or any type of stereotypical adornment. The room does not display academic titles, awards or professional achievements, as the focus is on the patient’s needs. During the interview, the doctor does not use a computer or any other type of device that obscures or diverts direct visual contact with the patient. A relaxed dialogue is initiated, giving the patient the necessary time to express their problems, doubts, insecurities and expectations. When the patient brings in exams, the physician reserves a later time to review them, without taking away from the humanized focus of the first consultation. After the evaluation, a physical examination is performed in another room, providing the necessary privacy for the patient. The time spent preparing and transporting the patient can be used by the physician for a preliminary analysis of laboratory and imaging tests. Upon returning to the interview room, the physician gives the patient and family his initial impression and describes the plan.
An effective doctor-patient relationship only occurs when the patient plays the protagonist and the doctor is the supporting actor
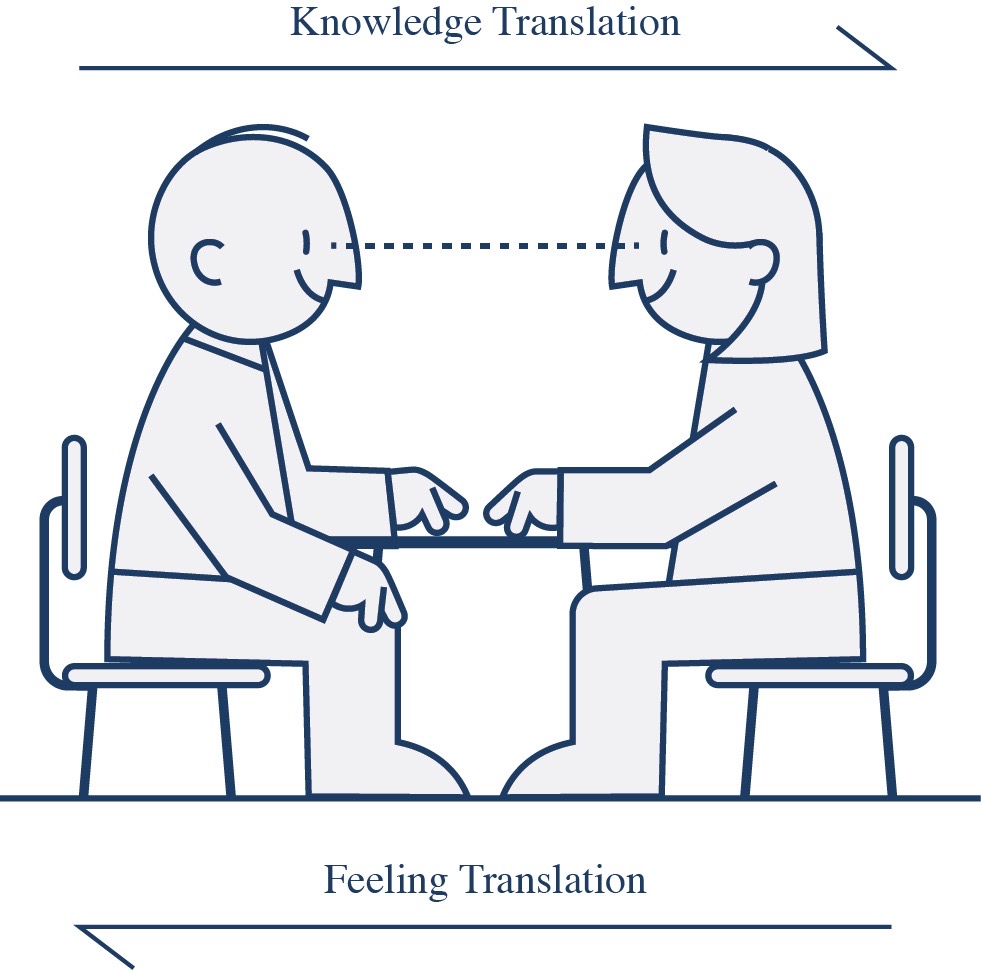
Looking at the circular care model shown in the figure below, it is difficult to identify who the doctor is. Well, this is the goal, because the relationship should be equitable. The members of the circular model know their roles and interact freely in an open and objective dialogue. The doctor holds the technical knowledge, but the patient and their family need to clearly understand the proposed intervention in order to qualify shared decision-making. Educational material is provided to the patient and their family members to understand how doctors think. To access it, click on the link above.

In the circular model, it is difficult to know who the doctor is, as their interface with patient and families must be equal
SHARED DECISION-MAKING
Practice of medicine is essentially centered on the doctor-patient relationship. All interventions are supported by levels of evidence, which must be adjusted to the needs and rights of the patient. Empathy, manifested in body language and clear speech, is essential for the success of the proposed interventions. The patient must clearly understand the recommendation, and the doctor must carefully guide a qualified decision-making process. Many clinical interventions are dictated by algorithms and a therapeutic index expresses their cost-benefit ratio. Informed consent only exists when the doctor is certain that the patient has fully understood the extent of the disease and the meaning of recommendations.
Shared decision-making is only reliable when the patient fully understands the recommendation
Note in the figure that shared decision-making is a two-way relationship, involving the physician and the patient in a horizontal line of communication. Medical knowledge is a universal domain, classified into levels of evidence and degrees of recommendation. The physician must be neutral when transferring this knowledge to the patient. The patient supports his or her decisions in the relationship of trust and, optionally, seeks the opinion of family members or other professionals. It is essentially an exercise in perceptions, which, after being processed by the patient, are communicated to the physician.
KNOW THE STEPS OF YOUR CARE
Here you will understand how we organize your care program. From the first contact, you will be interacting directly with the doctor, speeding up and customizing your care. Follow the step-by-step process and see how simple it is.
Step 1 | video conference

You will be guided to schedule a videoconference. By doing so, you are actively seeking to connect with your doctor. The virtual meeting facilitates this preliminary interface, promoting empathy and belonging. By learning about your story, your doctor will begin to share a care plan with you, based on your specific needs and the principles that govern evidence-based medicine. Little by little, you will understand the scope of your care, initiating a cooperative doctor-patient relationship, essential for the exercise of a patient-centric care model.
Step 2 | face-to-face consultation

During in-person consultation, the doctor is already familiar with your clinical case and is ready to meet your specific needs. Bring all the tests you have already performed. Come with a family member, as our care program includes both the patient and family. Prepare a list of questions. A well-informed patient qualifies shared decision-making. The in-person meeting strengthens the doctor-patient relationship and allows for the physical exam. The doctor will then record your clinical data using an algorithm that has digitized clinical problem-solving methodology.
Step 3 | customized care team

Medicine is an exercise in collective intelligence, where the attending physician assumes the role of a conductor, coordinating the work of consulting physicians. The attending physician contacts all the consulting physicians needed for your comprehensive care, creating a personalized care team. Working together, the physicians consensually compose your personalized care program, which will improve adherence to recommendations. Below, you will discover how the attending physician creates your personalized care team.
CREATING A CUSTOMIZED CARE TEAM
Your care will require an attending physician and consulting physicians. The number of consulting physicians will vary depending on the complexity of your problem. Here, the attending physician will select from several subspecialties those appropriate for your comprehensive care. Your attending physician will create your customized care team.
Customized Care Team
Clinical Data Upload
Clinical Data Download
CREATING A CUSTOMIZED CARE TEAM
Your care will require an attending physician and consulting physicians. The number of consulting physicians will vary depending on the complexity of your problem. Here, the attending physician will select from several subspecialties those appropriate for your comprehensive care. Your attending physician will create your customized care team.
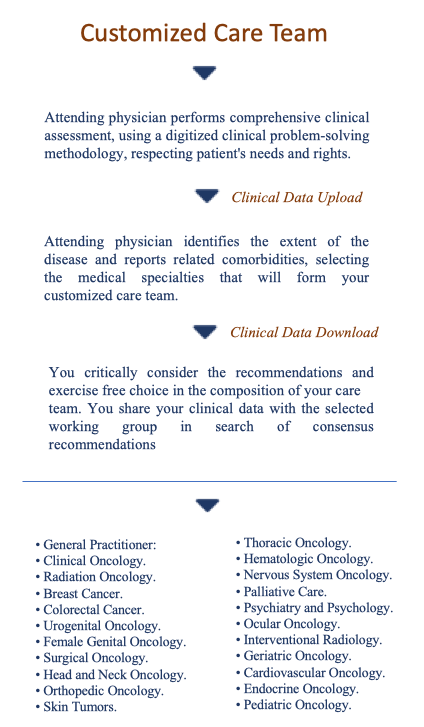
• General Practitioner.
• Clinical Oncology.
• Radiation Oncology.
• Breast Cancer.
• Colorectal Cancer.
• Urogenital Oncology.
• Female Genital Oncology.
• Surgical Oncology.
• Head and Neck Oncology.
• Orthopedic Oncology.
• Skin Tumors.
• Thoracic Oncology.
• Hematologic Oncology.
• Nervous System Oncology.
• Palliative Care.
• Psychiatry and Psychology.
• Ocular Oncology.
• Interventional Radiology.
• Geriatric Oncology.
• Cardiovascular Oncology.
• Endocrine Oncology.
• Pediatric Oncology.
Attending physician performs a comprehensive clinical assessment, using a digitized clinical problem-solving methodology, respecting patient’s needs and rights
Attending physician identifies the extent of the disease and reports related comorbidities, selecting the medical specialties that will form your customized care team
You critically consider the recommendations and exercise free choice in the composition of your care team. You share your clinical data with the working group and participate in the search for consensus
HOW WE ORGANIZE YOUR CLINICAL DATA
Your clinical data will be stored in a responsive Digital Health Record (DHR), which allows you to access it online on your computer, tablet or smartphone. You log in by choosing a unique username and password. This gives you immediate access to your DHR, making your health data available, in real time, anywhere in the world. The figure below shows the layout of your DHR. It is organized into 10 modules. When you hover your cursor over each module, it moves and its function appears in overlay.
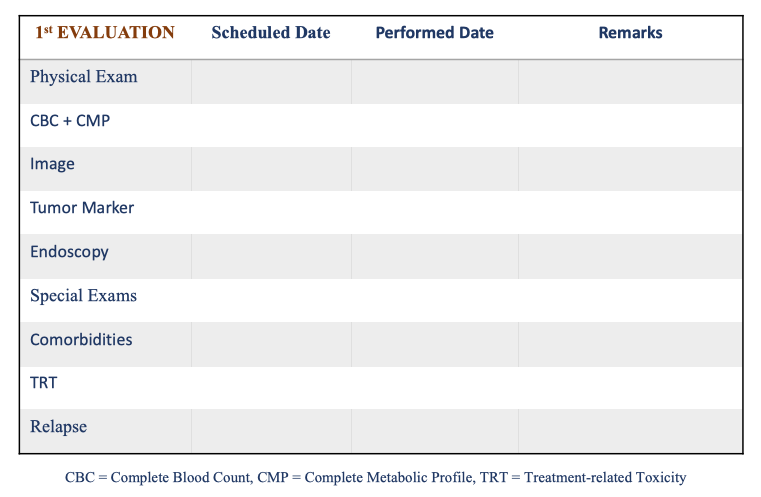
CUSTOMIZED FOLLOW-UP
To facilitate your care, a schedule is created, where you will receive a calendar of appointments. Your attending physician will fill it out, indicating the expected date of each intervention and the date on which it was actually performed. Remarks, when marked with (Yes), will be fully described in your DHR, indicating the need for further investigation.
See below a sample of your follow-up program: